How Technology is Revolutionizing eClinical Platforms
August 13, 2019
An academic article published on npj Digital Medicine shows that mobile technologies like smartphones, smartwatches, implantables, and similar are becoming more ubiquitous in clinical research. Sixty-seven percent of these technologies were categorized as wearable sensors.
This can only mean that technological adoption in the healthcare sector is high because they make it easier for researchers and clinicians to draw information from patients and subjects.
However, hardware is not the only technology sweeping across the healthcare industry. There are also technologies that synchronize one software with another and make research more flexible for all parties involved.
Here are some examples of how technology is changing the way we conduct clinical trials.
- Connectors for EDC & CTMS integration
System or software integration occurs when you connect different systems to create a coordinated assemblage. This is a common situation especially in SaaS platforms to streamline the flow of information between various interfaces.
Clinical trials can benefit from this because it reduces data entry. Since one solution can draw information from another, there is no need to input the same set of records again. What’s more, this keeps data accurate and ensures that no errors arise down the road.
This is possible because of connectors. These can be a separate entity from the main platform or it can be a built-in tool. Whichever the case, these ease the exchange of information between systems and clinical teams.
For example, a clinical trial management system (CTMS) can interface with an electronic data capture (EDC) technology. Because of this, users only have to use the latter to create records, saving time from rigorous data entry.
2. Interoperability for comprehensive clinical management
Interoperability can be easily confused with integration. However, for an eClinical platform, this means that the output of one system can be used in another solution. This structural interoperability is something that you can commonly encounter in a health ecosystem. That is because this preserves information in the course of data exchange with the help of standardized formats.
With this technology, you can take your records from one CTMS software to another without experiencing data loss, reformatting, or alteration in any form. Thus, you would not have to worry about throwing away invalidated records or conducting tests again.
Furthermore, interoperability expedites the submission of data to regulators. Your system may not be the same or integrated with that of the governing body’s, but with interoperability, you can save yourself the headache of preparing reports for authorities.
3. Real-time data refresh for up-to-the-minute information
When something happens in real time, it means there is no delay between the time of an event and the time you perceive this event. In clinical trial tools, this translates to instant access to new information as soon as it enters the system.
Because of this, you can be confident that you are working on the latest information in moving on to the best steps of a study. This is particularly critical when working with patient records or EMR. This enables your team to be more collaborative and proactive in ensuring the well-being of your patients and in adapting to the changing needs of subjects, physicians, and researchers.
Moreover, real-time data offer greater visibility into an eClinical trial and in the use of resources. As a result, decision-makers can make choices that can optimize operations.
4. Cloud technologies for convenient access
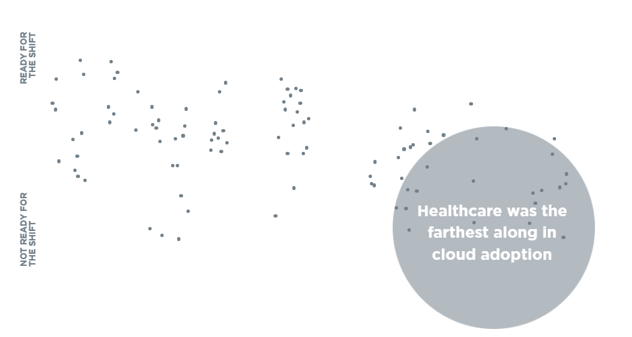
While many cloud applications available are focused on helping SaaS business to generate leads, it is actually the healthcare industry that has the most users of cloud technologies. In fact, it leads cloud adoption with 35% of healthcare organizations placing more than half of their records in a cloud platform.
Other than that, Becker’s Healthcare cites a survey conducted by West Monroe Partners, also found that many health organizations involved in the study moved to the cloud for better protection against data breaches and for lower maintenance costs.
A West Monroe Partners survey revealed that between financial, healthcare, and energy and utilities, the healthcare sector leads the way when it comes to cloud adoption.
Apart from stronger security and reduced IT expenses, cloud technologies offer other benefits such as the convenience of access. Since healthcare applications are in the cloud, patients can relay information about their physiological or psychological states to researchers wherever they are. This prevents delay in the collection and analysis of data on the part of clinical workers. This way, research institutions and healthcare organizations complete clinical trials faster.
5. Adaptive configuration for screen flexibility
One configuration that works for all screens is beneficial for both clinical trial researchers and their patients. Since they would have to set up systems from one device only once and see it on other platforms, investigators could focus more on gathering research data and processing them. Meanwhile, this would remove the limitation from trial subjects of working only with their computers to relay data to clinicians.
This is also advantageous because this prevents system errors due to incompatible configurations.
How to increase technology adoption in your organization
Not everyone in your institution may be open to new technologies. This can happen because they are not fully aware of the benefits these advancements bring. Plus, they may not be well versed in technology, which is why they are hesitant. The best way to approach this problem is to inform them of what the technology is, what it does, and how it can revolutionize their work. This way, you can ease them into adopting new technologies and ensure that they maximize them in their works.



